
Prior Authorizations Platform
The smart + simple way to manage prior authorizations
Prior authorizations are a leading cause of denied claims year after year— a problem that costs healthcare providers millions. What’s more, a lack of prior authorization solutions keeps patients from getting the care they need when they need it.
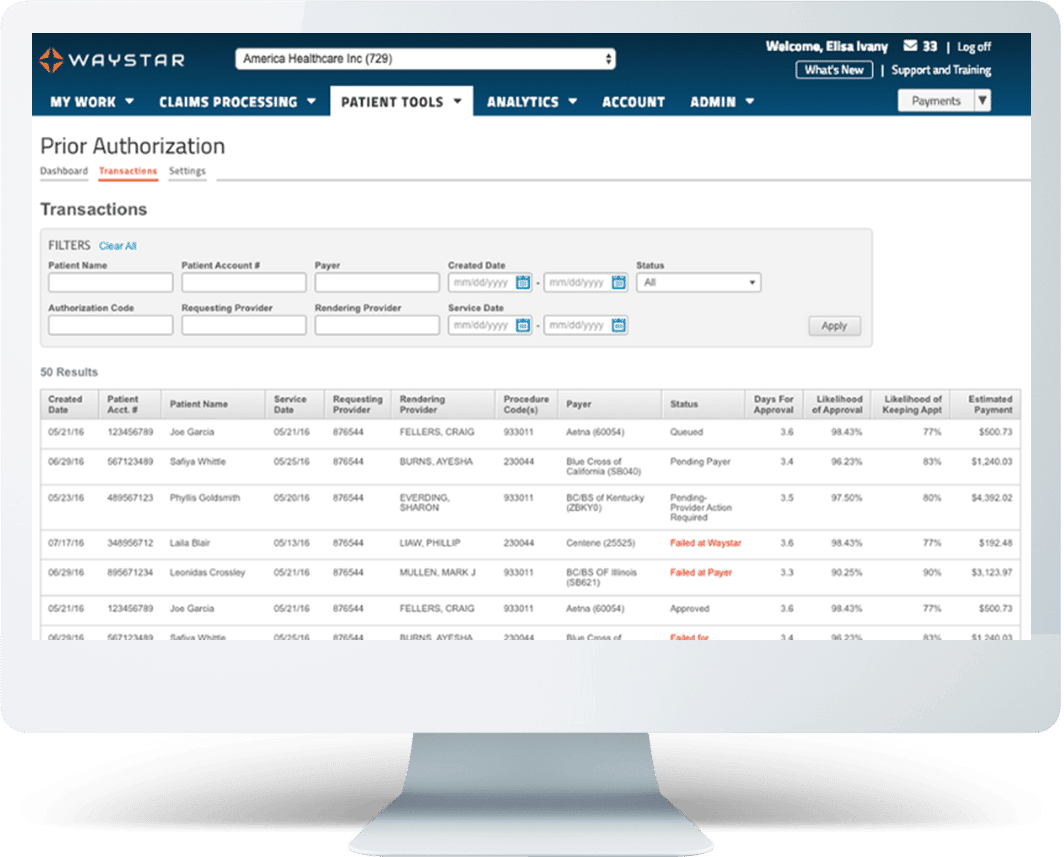
Waystar’s Prior Authorization Platform uses artificial intelligence and RPA to automate the authorization process from verification to status retrieval. Our prior authorization solutions automate not only authorizations, but notifications of admission, full-service medical necessity checks, and referrals. Clients have seen reduction in denials, and more efficient use of staff. Find the way forward.
Waystar’s Prior Authorization Solutions
Reduce denials + cut out manual work
Powered by intelligent automation, Waystar’s Prior Authorization solution:
- Automatically verifies, initiates, statuses, and retrieves comprehensive authorization details
- Initiates authorizations, saving time on manual processes
- Automates patient referral status to cut manual work, stop revenue leakage, and improve the patient experience
- Offers authorization submissions for unscheduled admissions
- Auto-generates Advance Beneficiary Notices or Notice of Non-Coverage forms for Medical Necessity
And, like all solutions that are part of our smart platform, Prior Authorization also:
- Integrates directly with all major HIS and PM systems
- Adapts to constantly shifting payer rules and requirements
- Is maintained by the in-house team of experts who built it

Prior auth by the numbers
How Prior Authorization works


WHAT MAKES WAYSTAR DIFFERENT
A prior authorization solution for faster approvals + lower costs
Waystar’s breakthrough prior authorization technology integrates with all major EMRs and payer systems, constantly working behind the scenes to gain speed, reducing turnaround time, and increase accuracy with every exchange. Our smart platform uses millions of rules, created with data from the millions of authorization transactions we conduct each year. And our RPA connectivity automatically routes authorizations to payers based on patient type and managing entity.
Find the way forward — for you and your patients.
Products included
Includes Prior Authorizations (initiate + status) | Medical Necessity | Admission Notification/Submission | Referrals
PRIOR AUTH RESOURCES
Get greater insights into prior authorization
Prior authorization 101
See the latest blogs on prior authorization
5 most unproductive touches in healthcare RCM
Atlantic Health reduces auth submission time by 50%+

Connect with an expert about our Prior Authorization Platform
Looking for more information on how Prior Authorization can speed approvals and cut costs? Fill out the form below, and we’ll be in touch shortly.